Abstract
Introduction:
HTLV-1 related adult T-cell leukemia-lymphoma (ATLL) remains fatal, thus urging development of new therapies. Interferon regulatory factor 4 (IRF4), also known as MUM1, is a transcription factor expressed in various aggressive B-cell and T-cell lymphomas (1). IRF4 has been reported to be highly expressed in HTLV-1 transformed cells and in aggressive leukemic forms of ATLL, and has also been implicated in interferon resistance. However, IFR-4/MUM1 expression, and its pathogenic role in ATLL have not been fully investigated. We previously reported lack of IRF4/MUM1 in leukemic ATLL specimens from patients who responded to AZT-interferon-alpha (AI). In this study, we characterized the expression of IRF4/MUM1 in our expanded ATLL cohort.
Methods:
ATLL specimens from 73 chemotherapy naïve patients of all subtypes [lymphomatous (L) n=31, acute (A) n=36, unfavorable chronic (UC) n=5, and smoldering (S) n=1] were analyzed for MUM1 expression. Cases were analyzed or confirmed by immunohistochemistry at our institution using anti-human MUM1 antibody (Dako) on formalin-fixed paraffin-embedded tissue or cellblock sections prepared from cytospun CD4+-enriched leukemic samples. The cutoff positive value for MUM1 expression was 30%. MUM1 expression was correlated with treatment outcome.
Results:
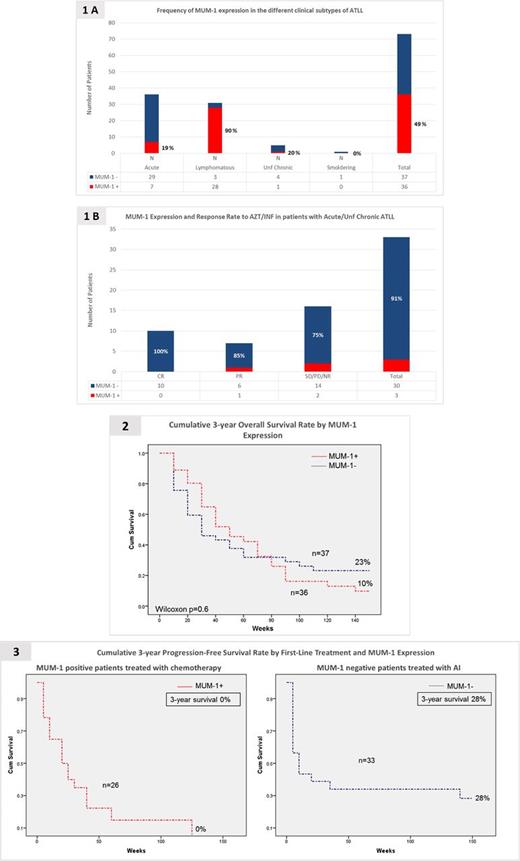
In 73 patients the proportion of MUM1+ cases was as follows: L (28/31 =90%), A (7/36 =19%), UC (1/5 =20%), and S (0/1 =0%) (Figure 1A). MUM1 expression was analyzed in 33 chemotherapy naïve patients with A (n= 28) or UC type (n=5) treated with AI; only 3 patients (A n=2, and UC n=1) were MUM1+ and had partial response (PR) (UC n=1), stable disease (SD) (A n=1), and no response (NR) (A n=1) respectively (Figure 1B). All 9 patients who achieved a complete response (CR) (A n=7, and UC n=2) and 6 patients with PR (A n=5, UC n=1) were MUM1-. The cumulative 3-year overall survival (OS) rates in MUM1- (n=37) vs. MUM1+ (n=36) patients were 23% vs. 10% respectively (p=0.68) (Figure 2). Notably, the great majority of patients in the MUM1- group (33/37=89%) were treated with AI as first line therapy and were A-type (27/37=73%), while most patients in the MUM1+ group (26/36=70%) were treated with chemotherapy upfront and were L-type (23/36=64%). The cumulative 3-yr progression-free survival in MUM1- patients treated with AI was 28% as compared to 0% in MUM-1+ treated with chemotherapy (Figure 3).
Conclusion:
Our results demonstrate that MUM1 expression is highly associated with L-type ATLL. Patients with aggressive leukemic ATLL subtypes treated with AI generally lacked MUM1 and had a significant better outcome than L-type patients treated with chemotherapy. This study suggests that MUM1 expression may influence the biology at ATLL subtypes and response to interferon-based therapy. Targeting IFR-4/MUM1 function in L-type ATLL should be considered as a therapeutic strategy. The analysis of additional cases is still ongoing and the final results will be presented at the meeting.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.